In the United States there are about 270,000 cases of Breast Cancer each year, and 99% of them are in women. If you are a woman, and you live to 80, you have a 1 in 8 chance of developing breast cancer during your lifetime. Today’s post provides updates on breast cancer, BIA-ALCL and BIA-SCC.
Breast Cancer Risk Factors
Women with larger breasts seem to be at higher risk of breast cancer. In fact, Breast Reduction Surgery is associated with a reduction in the risk of breast cancer; however, there are more important risk factors to discuss. The top three breast cancer risk factors are:
- Age
- BRCA1 and BRCA2 gene mutations
- Breast Density
Breast Cancer and Age
Older age is the greatest risk factor for breast cancer, with the sole exception of being born female. The rates of diagnosis climb as we age, and do not peak until the mid 70’s. The diagnosis of breast cancer is possible at any age, but is more common after puberty. This may be due to increased hormone levels. Delayed childbirth and late menopause also increase the risk, likely from the longer period of hormone exposure. Other risk factors increase as we age such as obesity, smoking, alcohol, certain medications and low levels of Vitamin D.
White women have the highest rate of cancer (515 per 100,000) followed by black women (460 per 100,000). Black women, however, have the highest death rate from breast cancer (193 per 100,000), followed by white women (183 per 100,000). The truth is, breast cancer affects all women, regardless of ethnicity, in large numbers. The lowest risks are seen in Asian/Pacific Islanders, with the incidence reduced by one third and the death rate by one half. 10% of breast cancer occurs in men, and it is usually more advanced at the time of presentation.
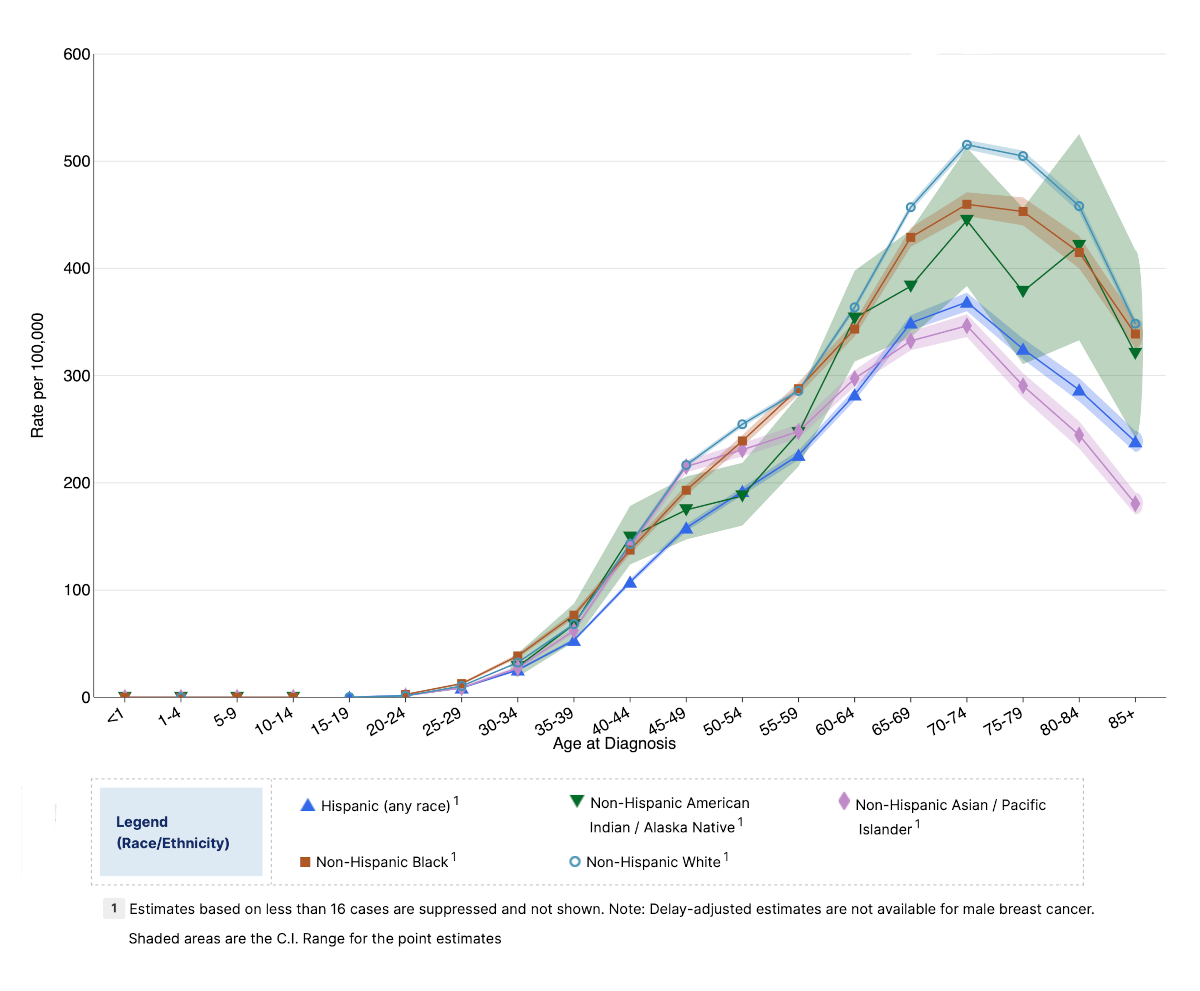
Age is the greatest risk factor for breast cancer. The rates climb as we age, and do not peak until the mid 70’s. White women have the highest rate of cancer followed by black women. Black women, however, have the highest rate of death from breast cancer.
The above graph was created on the NIH’s National Cancer Institute website. If you want to play with it, here is the link to the graph. On the site you can choose from many options: types of cancer, age, sex, ethnicity, incidence, prevalence, trends. Moreover, you can view the raw data and get additional information by hovering over any point. By the way, the data still shows 40 is the right time to get your first mammogram, unless you are at higher than average risk.
Breast Cancer and Genetics
A family history of breast cancer increases your risk of developing breast cancer. Your risk of breast cancer doubles if your mother, sister or daughter have had it. On the other hand, 80% of all breast cancer patients have no family history.
Gene mutations, such as BRCA1 and BRCA2, are recognized as high risk factors for breast cancer. Like all science, it is about odds rather than predictions. About one in 500 women in the US have either a BRCA1 or BRCA2 mutation. This is not a death sentence; however, the risk of breast cancer in women with a mutation in BRCA1 or BRCA2 genes is estimated at 60% to 85%. The risk of ovarian cancer in these women is estimated at 15% to 60%. Other genes are involved and other factors come into play.
Breast Cancer and Breast Density
Breasts are considered dense if they have more glandular tissue and less fat. This is more common in younger women, as breasts become more fatty as we age. Breast density is also inherited and a risk factor for breast cancer. One possible reason for this is that dense breast tissue contains more breast cells, just like larger breasts. It’s just that the cells are more compacted together. Only age and BRCA gene mutations are more closely associated with the formation of breast cancer.
Breast Implant Associated Cancer
In recent years, BIA-ALCL and BIA-SCC, have received attention in the press and the FDA. It is important to remember two things. These are not breast cancers, and both are very rare when compared to breast cancer.
Last year, in the US alone, almost 300,000 women were diagnosed with breast cancer and 40,000 women died of breast cancer. This is why doctors insist on getting routine mammograms and appropriate follow-up care.
In the history of breast implants, between 1963 and 2023, there have been fewer than 1400 cases of BIA-ALCL reported and fewer than 20 cases of BIA-SCC reported world wide. Let’s briefly review both.
Breast Implant Associated Large Cell Lymphoma (BIA-ALCL)
Breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) is not breast cancer. It is an uncommon and treatable type of T-cell lymphoma that can develop around breast implants.
The American Society of Plastic Surgeons (ASPS) is the leading authority in BIA-ALCL. The ASPS recognizes approximately 411 both suspected and confirmed cases in the United States and nearly 1,400 cases worldwide as of March 2023.
The average age of presentation is 55.3 years, and the average length of time after initial breast augmentation is 10.32 years.
The tumor is associated with textured breast implants. No cases of BIA-ALCL have been confirmed in patients who have only had smooth implants in case series, case reports or registries. However, I am sure a case will eventually be found.
BIA-ALCL is more commonly found in women of Northern European descent, even though a smaller percentage of them have textured breast implants. Textured breast implants are used more often in Asian countries, but the incidence of BIA-ALCL is much lower in this population.
The most common presentation is fluid around the breast implant, causing swelling, pain and redness on the involved side, though other causes of these symptoms are more likely. 28% of patients have extracapsular spread; however, the most common presentation is a mass confined to a single area on the capsule. Fluid sampling for CD30+ and ALK-, flow cytometry for T-cells and ultrasound are the first steps toward diagnosis.
Treatment will depend on the details of each case, but removal of the implant and capsule (en bloc) are usually recommended.
Breast Implant Associated Squamous Cell Cancer (BIA-SCC)
Breast implant associated squamous cell cancer (BIA-SCC) is extremely rare. This type of tumor can be found with any implants, such as hip replacements or dental implants.
According to the ASPS, there are 19 cases of BIA-SCC reported in the literature. Average age of presentation is 55.8 years, and the average length of time after initial breast augmentation is 22.74 years.
BIA-SCC is associated with both textured and smooth breast implants.
It commonly presents as swelling, pain and redness like BIA-ALCL; however, unlike BIA-ALCL, BIA-SCC is often associated with capsular contracture and has an incidence of extracapsular spread of 80%.
Fluid sampling for CK 5/6+ and p63+, flow cytometry for squamous cells and keratin and ultrasound are the first steps toward diagnosis.
Due to its rare nature, treatment for BIA-SCC is evolving. It appears that explantation with aggressive (en bloc) capsulectomy provides the best outcomes. Based on existing case reports, it appears that incomplete resection of BIA-SCC can result in early and/or aggressive recurrence.
More information is available on the ASPS website here: FDA provides update on Breast Implant Associated-Squamous Cell Carcinoma (BIA-SCC)
Previous Post Next Post